With funding from the Engineering and Physical Sciences Research Council (EPSRC) and in collaboration with St Thomas’ Hospital, a team at King’s College London has taken the first steps in developing models designed to optimise a procedure that corrects atrial fibrillation, a condition which causes abnormal heart rhythms.
The new personalised computer models aim to increase the effectiveness of this procedure (which is known as ‘catheter ablation’) by making it possible to explore, in advance, different strategies for its use geared to the specific needs of individual patients. They could potentially save the NHS over £20million a year by reducing procedure times and cutting atrial fibrillation recurrence rates.
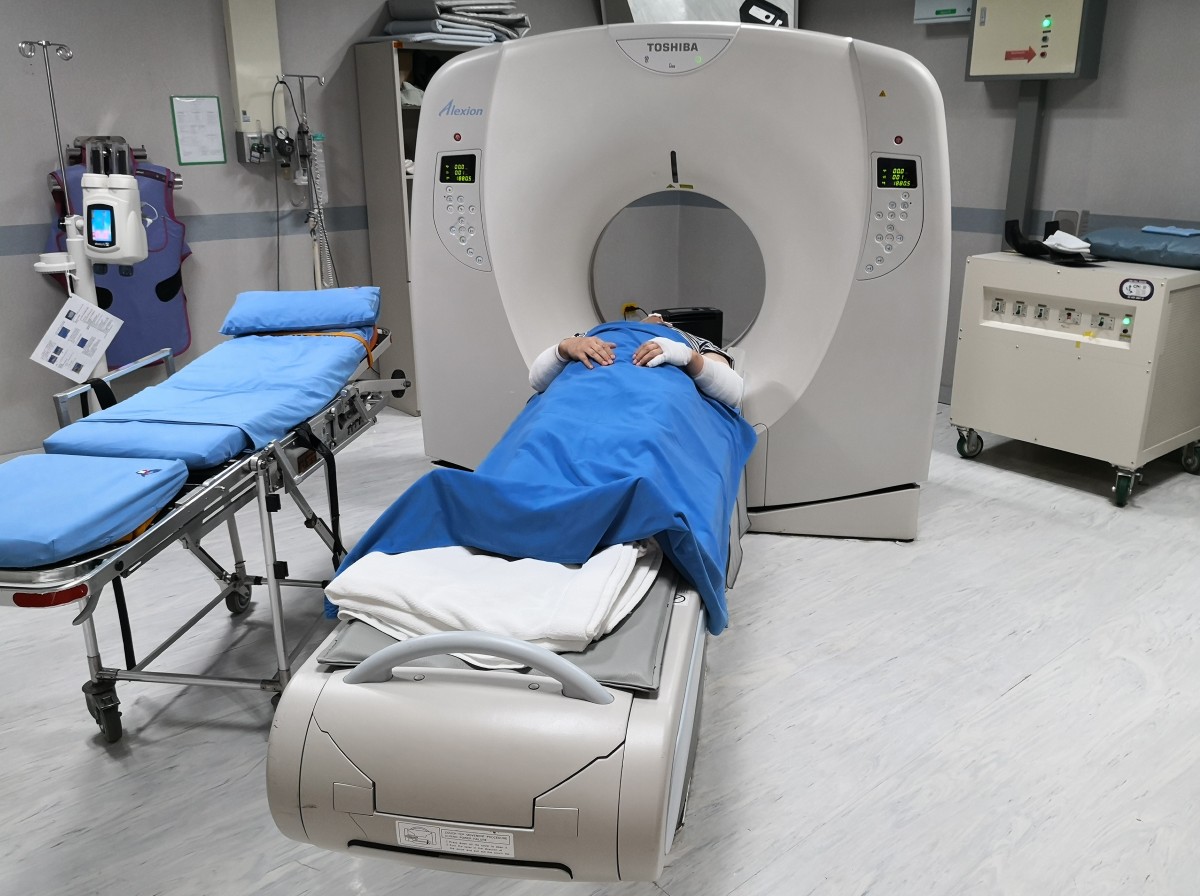
Atrial fibrillation reduces blood supply, leading to dizziness, breathlessness and fatigue, and increases the risk of a stroke. Every year, around 10,000 people in the UK have a catheter inserted in order to treat the condition using radiofrequency energy. But the procedure is not always effective, there is a small risk of it causing a stroke or death, and the condition often recurs.
Developed using skills in computational modelling, software development and image processing, and based on detailed data about the patient’s heart obtained through medical imaging, the models depict tissue condition and blood flow, and enable simulation of around 10 cardiac cycles lasting a few seconds in total.
Dr Adelaide de Vecchi of King’s College London, who has led the project, says: “The really important thing is that these new personalised models show the heart working as a whole 'system'. They allow different catheter ablation strategies to be assessed for each specific patient – for example, with regard to the precise area of the heart to target – and therefore enable the very best option to be pinpointed, maximising the prospect of improving the patient’s quality of life.”
The models have been tested in collaboration with Dr David Nordsletten, Dr Oleg Aslanidi and Dr Des Dillon-Murphy from King’s, using clinical data from patients under the care of Professor Mark O’Neill at St Thomas’. The aim is now to enhance and extend the models in terms of the number of cardiac cycles they can depict and apply them to larger cohorts of patients. Once this is achieved, it is anticipated that full clinical trials will be undertaken.
Dr de Vecchi says: “Subject to further development, we believe our models have the potential to enter routine clinical use within a decade, improving treatment of a condition that is especially common among older people. The models are very much in step with the drive towards personalised medicine, better cardiac care and improved management of our ageing population.”